This is the first in an ongoing series to help care providers, including Ontario Health Teams (OHTs), advance the province’s Digital First for Health strategy
by Dr. Jeff Alfonsi, MD, FRCPSC
Digital technology is transforming our world. Today, the virtual is vital—in almost every aspect of our lives. Health care is no exception.
In Ontario, where the government is introducing a new integrated, patient-centred delivery model, there has been a lot of buzz about how virtual care can assist overall system transformation. Under newly formed Ontario Health Teams (OHTs), health care providers—including hospitals, physicians, home and community care providers, and others—will work as coordinated teams, no matter where they deliver care. The desired goal? To strengthen local services, making it easier for patients to navigate the system and transition between providers.
The face of health care delivery is changing quickly, and this pace will continue. In mid-November, Ontario Health Minister Christine Elliott announced a new Digital First for Health strategy in addition to previous guidelines that between two and five percent of OHT patients should have a virtual health care encounter in the team’s first year. The new strategy is built on five “pillars” which, when fully implemented by 2021-2022, will offer more virtual care options, including:
- expanding secure messaging and video visits (55,000 more of which will be provided by Ontario physicians to patients over the next year)
- expanding access to online appointment booking
- providing more secure access for patients to their online health records
- offering better, more connected tools for frontline providers to securely share information and
- enhancing data integration and predictive analytics
So, if virtual care has not previously been on your radar, or even if you have already adopted a virtual care model, it is time to start thinking about how virtual care can further enhance care delivery. It’s not just a target in and of itself, it’s a means of achieving broader integrated health care goals.
The Ministry of Health has stated its new strategy “will harness the imagination and capabilities of Ontario’s digital health innovators to improve care for all Ontarians.” That will require even greater collaboration and knowledge sharing. Evidence clearly shows that virtual care can significantly support both clinical and business objectives. For some inspiration, check out some model of care profiles that show how virtual care can help address challenges, how it can be integrated into workflows, and what impact organizations are seeing as a result.
What Exactly is Virtual Care?
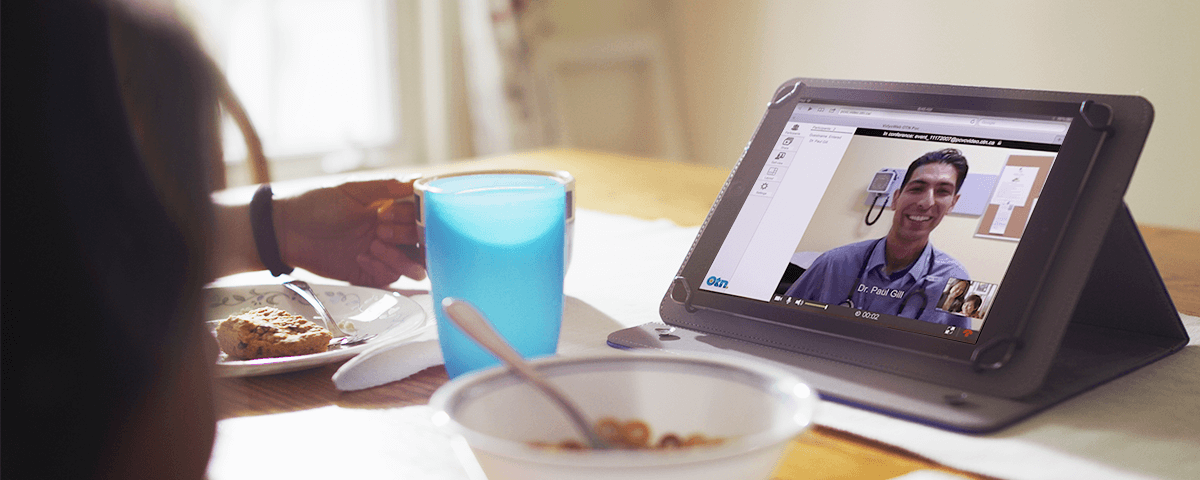
Virtual care is defined as an electronic exchange (i.e., not in-person) between providers and patients, and between providers, concerning one or more health issues or concerns. Virtual care can happen in real time, which is referred to as synchronously, or asynchronously.
Synchronous encounters often leverage videoconferencing. For instance, a patient with debilitating agoraphobia could see their psychiatrist from the comfort of home, which is not just a convenience but also a reassurance. Other cases include post-hospital discharge follow-up for older patients who may have trouble travelling to a clinic, or for a hospital struggling with limited ambulatory space or available appointments.
Asynchronous encounters may include secure messaging between providers and patients and their caregivers, remote monitoring, and online advice-sharing between providers. For example, the Ontario eConsult Program enables primary care providers to directly ask a specialist online questions about care so that they can build their knowledge and continue to support their patient without the need for an in-person specialist visit. Responses are received between two to three days.
Many technologies support virtual care delivery and more are on the way. They include videoconferencing, secure messaging, wearables, mobile applications—including sensors, microphones, and accelerometers—as well as peripherals, such as Bluetooth-enabled blood-pressure cuffs, scales, and other monitoring devices.
We’ll explore the keys to success to virtual care integration—both pitfalls and enablers—in later installments of this series. We’ll also take a closer look at the virtual care landscape, including policy implications, and how to identify current-state virtual-care use in your region, solutions to meet the needs of your target patient populations, and how to effectively implement virtual care. So please stay tuned, explore the many resources available through otn.ca to support virtual care uptake, and reach out to us at any time to share knowledge and explore opportunities to work together to deliver better care.
Dr. Jeff Alfonsi, MD, FRCPSC, is an Assistant Professor at Western University and Director of Medical Affairs at OTN.
Up next: Exploring effective models of care, in Ontario and globally
